“HUSF Hospital in Brazil Implements Circle Up (“The Team Circle”) Fostering a Culture of Teamwork and Psychological Safety”
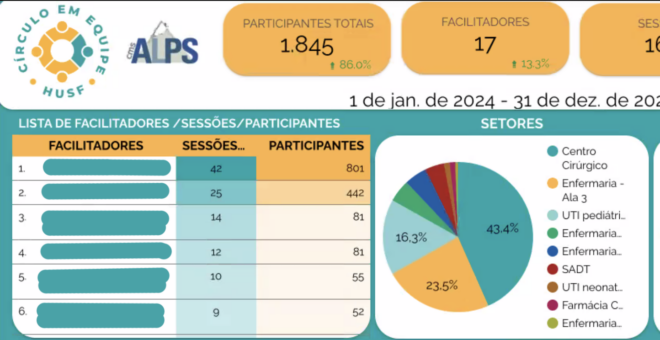
The Hospital Universitário Sagrada Família (HUSF) in Araguari, Brazil, with the assistance of CMS Affiliate Master Education Institute President Antonio Carlos (IMEPAC), has taken a significant step…

