Dr. Lon Setnik, Emergency Physician and Medical Director of the Forrest D. McKerley Simulation and Education Center at Concord Hospital is working to help keep patients and staff safe during the Coronavirus (COVID-19) outbreak. Dr. Setnik created the COVID-19 Suspected or Confirmed Airway Management Checklist to assist with team organization and preparation when faced with the need to intubate a patient.
Intubation during the COVID-19 outbreak is one of the more dangerous procedures for our teams. We worked across the organization to create an approach that would keep our patients and providers as safe as possible during this pandemic.
The COVID-19 Suspected or Confirmed Airway Management Checklist is designed for the team to use outside the room as they set up for managing the airway, and inside the room to remind them how their job should be performed in this new process.
COVID-19 Suspected or Confirmed Airway Management Checklist
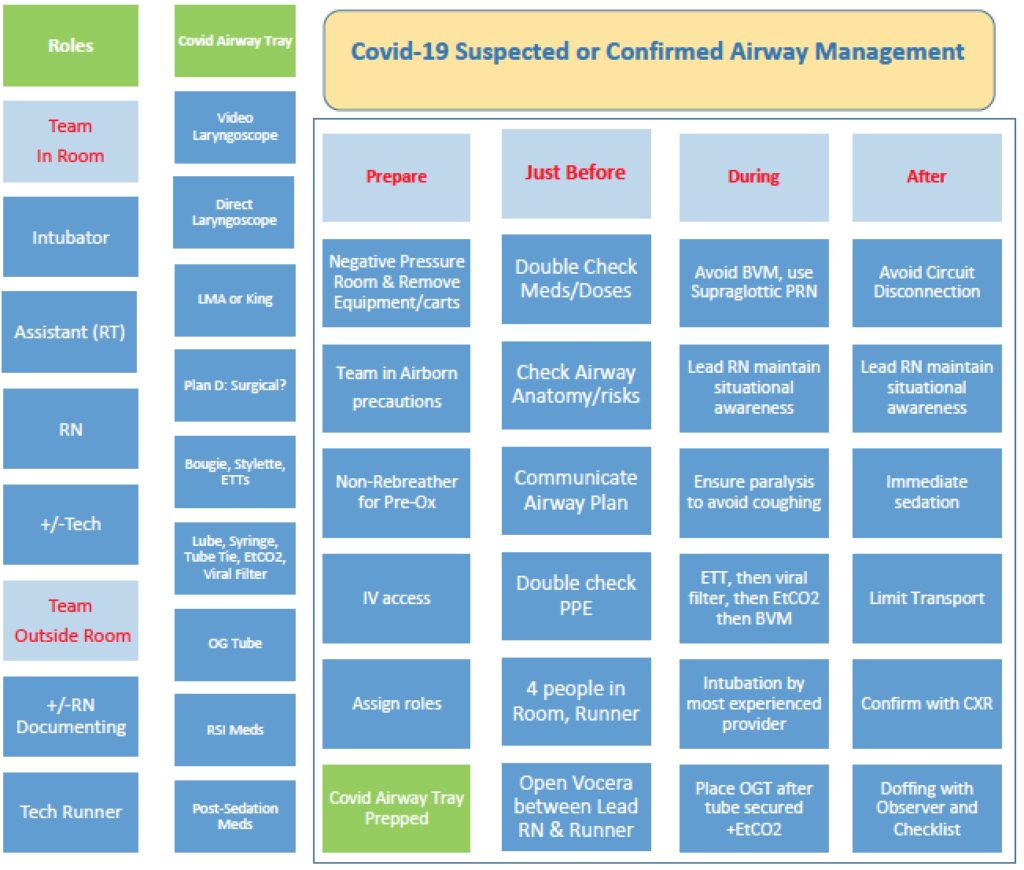
First the Roles are assigned (left column).
Then the Airway Tray (second column) is set up while the team members are donning appropriate precautions.
The “Just Before” column is designed to have the team perform a brief “Time Out.” Our organization uses Vocera which is a hands-free communication device. It can be finicky to start a call so we do this before any emergency develops. A cell phone could alternatively be used. This also allows the nurse outside the room to document even though the door is closed, so no paper is in the room.
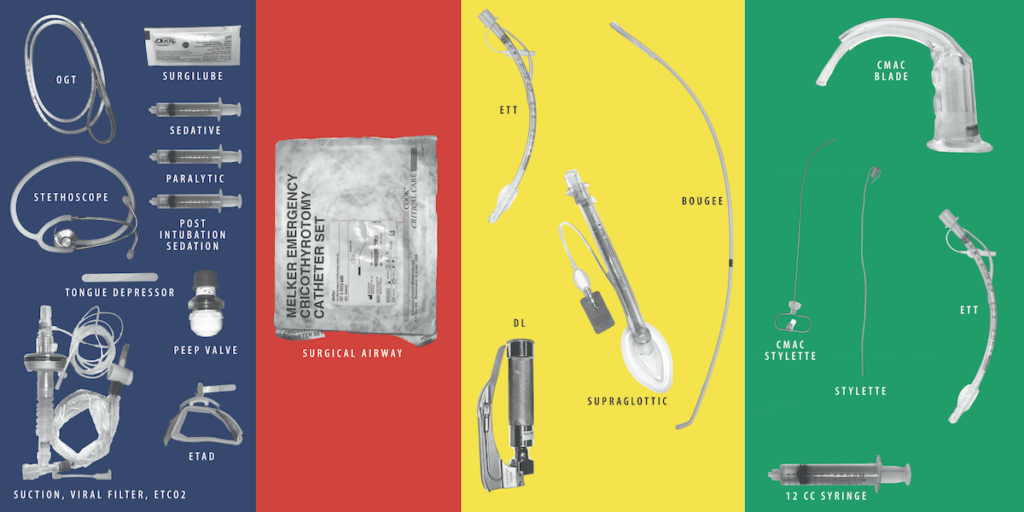
The Airway Map
The Airway Map (pictured above) is a printed/laminated (cleanable) 30×14 inch sheet that is used to ensure the team has everything they need before they enter the room. It is designed to fit on a standard bedside table although we have larger tables in the resuscitation bay. Green is plan A, yellow is Plan B and a rescue device, red is plan C. Some providers want different equipment but this is a way for them to have the conversation with the team before they are fully donned, and to reduce the need to have the entire airway cart or bag in the room, which is not allowed because of possibility for contamination.
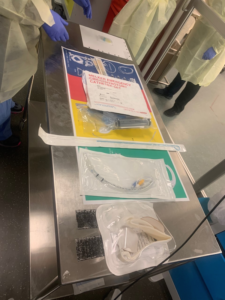
Here’s an image of the first time this was put to use, we printed on plain paper to ensure it met people’s needs for the first few times it was used.
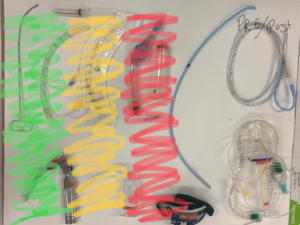
The V1, V2, and V3 images below demonstrate the iterations we went through over the first week, working with anesthesiology and ICU teams to develop a relatively standard process and mental model for anyone who might need to intubate anywhere in the hospital.
After we had a relatively stable version we had our PR department create the images for the final version, and I’m grateful for Sam Mostue for his work to get this done so quickly.
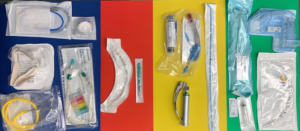
We have also updated our portable airway box that we might need to bring to the units to intubated to include baggies containing the needed equipment to populate the map, an early prototype shown below.
This allows us to have a team-based system of care with the resources they need during this dangerous procedure. This entire activity has brought our intubation teams closer together, including respiratory therapy, nursing, patient care technicians, and the departments of intensive care and anesthesiology. We have also observed improved role clarity during the intubation by creating this process.
Please let me know if you have any questions, or about the training rollout used, or meta-process to get us where we are. Many thanks to Albert Chan (@gaseousXchange) Christopher Hicks (@HumanFact0rz) and Cliff Reid (@cliffreid) and others for their twitter based feedback at many points. I have never talked to or met Chris Hicks or Cliff Reid, but they have been instrumental to me as a resource over the last 2 weeks.
I’m attaching the various sources I used to help create this Checklist and Airway Map.
https://drive.google.com/drive/folders/1a09DRlITYUieH43-VlFFULcgLc8kMX9p
https://twitter.com/gaseousxchange/status/1230097640496320513
https://twitter.com/humanfact0rz/status/1241859422059663360
https://twitter.com/cliffreid/status/1240436586824601600
– Lon Setnik, MD, FACEP